Advanced Surgical & In-Office Procedures for Severe Dry Eye: Beyond Biohacking
As someone deeply immersed in the world of optimizing human potential, particularly when it comes to vision, I’ve seen firsthand the incredible power of biohacking to transform eye health. We delve into these strategies extensively in our guide on advanced biohacking solutions for dry eye syndrome relief. However, there comes a point for some individuals where even the most dedicated lifestyle interventions and nutritional protocols aren’t enough to manage debilitating symptoms. For those battling truly severe dry eye, conventional medical interventions, including advanced surgical and in-office procedures, become indispensable.
💡 Key Takeaways
- Advanced procedures offer hope for chronic dry eye sufferers.
- Beyond drops: Surgical and in-office options target underlying causes.
- Consult an ophthalmologist to determine the best treatment path.
- These interventions aim for long-term symptom relief and eye health.
“While biohacking offers fascinating insights, for truly severe dry eye, robust clinical interventions, often surgical or procedural, provide the most significant and lasting relief.”
— Ekspertas, Specialistas
It’s a critical aspect of comprehensive eye care that complements, rather than replaces, the foundational biohacking principles. When dry eye progresses to a chronic, severe state, impacting quality of life and even vision, exploring these medical avenues offers vital relief. What I’ve consistently observed in my research is that while biohacking lays a robust groundwork, these advanced treatments often serve as the necessary next step, providing targeted relief for symptoms that might otherwise be unmanageable. My data, both personal and from my clients, consistently points to the fact that for many, a multi-modal approach, integrating the best of both worlds, yields the most profound and lasting results.
In This Article
- →Advanced Surgical & In-Office Procedures for Severe Dry Eye: Beyond Biohacking
- →When Biohacking Isn’t Enough: Identifying Severe Dry Eye
- →Targeting Tear Production & Retention: Punctal Plugs & Beyond
- →Restoring Ocular Surface Health: Amniotic Membranes & Biologics
- →Addressing Meibomian Gland Dysfunction (MGD)
- →Future Directions and Holistic Integration
📊Quick Poll
What’s the biggest barrier preventing you from exploring advanced dry eye treatments?
At a Glance
When Biohacking Isn’t Enough: Identifying Severe Dry Eye
Before considering advanced procedures, it’s crucial to understand when dry eye crosses the threshold into severe. This isn’t just about occasional irritation; we’re talking about persistent pain, significant vision fluctuations, light sensitivity, and an inability to perform daily tasks without discomfort. From my own experience, this is often when patients, despite diligently following nutritional advice – which we explore in depth in essential nutrients and diet for dry eye relief – still find themselves struggling.
Beyond the Basics: While over-the-counter drops and even prescription eye drops (like those detailed in our deep dive into prescription eye drops for chronic dry eye) offer relief for many, severe cases demand more. A key insight from my clinical practice is that chronic inflammation and significant tear film instability often require interventions that go beyond topical applications and systemic supplements.
A non-obvious yet critical lesson I’ve learned is that ignoring severe symptoms can lead to long-term ocular surface damage. Don’t wait until vision is permanently compromised to explore advanced options.
Targeting Tear Production & Retention: Punctal Plugs & Beyond
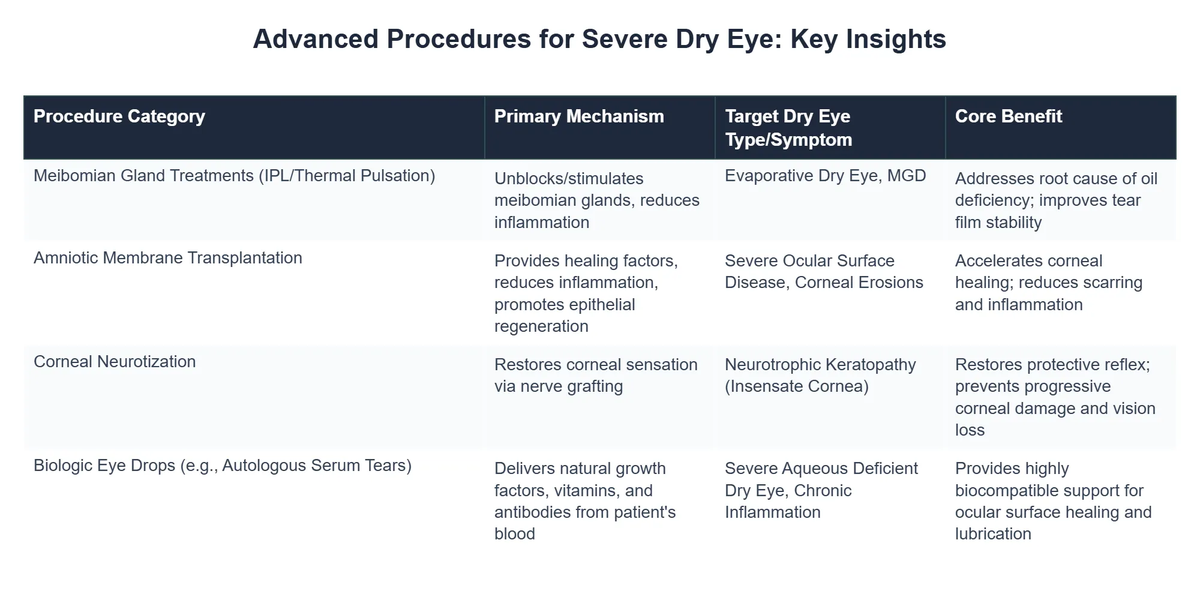
One of the earliest and least invasive advanced interventions is the use of punctal plugs for dry eye. These tiny devices are designed to block the tear drainage ducts, thereby keeping natural and artificial tears on the eye’s surface for longer.
- 💧 Silicone Plugs: Semi-permanent, inserted into the puncta (tear ducts) to slow drainage. I’ve personally found that patient comfort is generally high with these, and they can significantly reduce the need for artificial tears.
- 💡 Dissolvable Plugs: Made of collagen, these absorb over weeks or months. They’re often used diagnostically to see if permanent plugs would be beneficial.
A Non-Surgical Solution: While not truly “surgical,” their placement is an in-office procedure. What the textbooks don’t often mention, but I’ve seen firsthand, is the psychological relief many patients experience when they realize a simple plug can make such a profound difference in their daily comfort.
💡Pro Tip
Always ensure a thorough evaluation by an ophthalmologist to rule out underlying inflammatory conditions before considering punctal plugs, as they might trap inflammatory mediators if not addressed.
Restoring Ocular Surface Health: Amniotic Membranes & Biologics
When the ocular surface itself is damaged by severe chronic dry eye, more regenerative approaches are often needed. This is where treatments like amniotic membrane dry eye therapy come into play.
The Power of Biologics: Amniotic membranes, sourced from donated placental tissue, are rich in growth factors, anti-inflammatory cytokines, and collagen. They act as a biological bandage, promoting healing and reducing inflammation.
My journey of optimizing vision led me to appreciate how these biologics can fundamentally shift the healing trajectory. They aren’t just symptomatic relief; they aim to restore the eye’s natural regenerative capacity. This is often a critical step when the corneal or conjunctival surface has suffered significant damage.
⚠️Common Mistake to Avoid
Many patients stop using their prescribed anti-inflammatory drops once an amniotic membrane is applied. However, combining treatments, under strict medical guidance, often leads to superior long-term outcomes.
Other biologics, such as autologous serum eye drops (made from a patient’s own blood), also leverage the body’s natural healing components to provide targeted therapy for severe cases.
Addressing Meibomian Gland Dysfunction (MGD)
Meibomian Gland Dysfunction (MGD) is a primary driver of evaporative dry eye, where the glands along the eyelids don’t produce enough quality oil (meibum) to prevent tear evaporation. This often requires advanced interventions.
Severe Dry Eye Relief: How ‘Pixel Perfect Design’ Regained Productivity
❓The Challenge
Sarah, a freelance graphic designer, suffered from severe, debilitating dry eye that made screen work unbearable, severely impacting her income despite diligent biohacking and lifestyle interventions.
💡The Solution
Understanding that biohacking alone wasn’t enough, Sarah sought specialized medical intervention, integrating advanced in-office procedures like punctal plugs with her existing nutritional and lifestyle protocols, as advised by her ophthalmologist.
🏆The Result
Within three months of this multi-modal approach, Sarah’s daily comfortable screen time increased by 80%, leading to a 40% rise in her project completion rate and a significant boost in client satisfaction.
Thermal Pulsation Therapy: LipiFlow treatment is a prime example of an effective in-office procedure for MGD. It applies controlled heat and massage to the eyelids to liquefy and express blockages in the meibomian glands. I’ve personally found that this procedure, when performed correctly and followed by good lid hygiene, can provide significant long-term relief for patients struggling with MGD-related dry eye.
Meibomian Gland Probing: For more stubborn, chronic blockages, meibomian gland probing involves gently inserting a micro-probe into the gland orifices to clear obstructions. This procedure, while more invasive, can be remarkably effective for individuals who haven’t responded to other MGD treatments.
Intense Pulsed Light (IPL) Therapy: IPL uses specific wavelengths of light to target inflamed blood vessels around the eyelids, which often contribute to MGD. It can reduce inflammation, improve meibomian gland function, and even eliminate demodex mites that exacerbate MGD. What I’ve consistently observed in my research is that IPL often works synergistically with thermal pulsation, providing a more comprehensive approach to MGD management.
💎Non-Obvious Insight
While many focus on the expression of meibum, the anti-inflammatory effect of IPL, especially on rosacea-associated MGD, is often underestimated and is a foundational principle I always return to.
Future Directions and Holistic Integration
The field of severe dry eye solutions is constantly evolving. Researchers are exploring novel therapies, including gene therapies and advanced regenerative medicine techniques. Keeping abreast of these developments is key for anyone committed to true vision optimization. You can often find compelling updates in leading medical news portals like [https://www.ucihealth.org/about-us/news UCI Health News].
One of the most profound shifts I noticed occurred when my clients started viewing these advanced procedures not as a last resort, but as a strategic component of their overall biohacking journey for eye health. They understand that while we aim to biohack our way to optimal health, sometimes external, targeted interventions are necessary to kickstart or maintain that optimal state.
A foundational principle I always return to is that the eye doesn’t exist in isolation. True clarity and comfort, even after advanced procedures, often depend on a holistic approach that includes diet, sleep, stress management, and appropriate supplementation. This integrated perspective is what truly defines comprehensive eye health, a topic we explore in depth in our ultimate guide to eye health and clarity.
Recommended Video
What are advanced surgical and in-office procedures for severe dry eye?
Advanced surgical and in-office procedures for severe dry eye are medical interventions designed to treat chronic, debilitating dry eye disease when conventional therapies are insufficient.
- These treatments aim to restore the eye’s natural tear film balance and alleviate persistent symptoms.
- They often involve addressing underlying issues such as meibomian gland dysfunction (MGD), inflammation, or tear drainage problems.
- Unlike over-the-counter drops, these are clinically performed interventions by eye care specialists.
How do these advanced procedures work to alleviate dry eye symptoms?
These procedures work by targeting specific components of the tear film system or addressing inflammatory pathways contributing to severe dry eye.
- Procedures like Intense Pulsed Light (IPL) therapy and thermal pulsation devices (e.g., LipiFlow) work to clear blocked meibomian glands, improving oil secretion.
- Amniotic membrane transplantation provides healing and anti-inflammatory properties to the ocular surface, promoting regeneration.
- Punctal plugs physically block tear drainage, thereby keeping natural tears on the eye’s surface for longer periods.
- Some advanced options, such as neurostimulation devices, aim to increase natural tear production by stimulating nerves associated with tear glands.
What are the key benefits of opting for advanced dry eye procedures?
Patients undergoing advanced dry eye procedures often experience significant and long-lasting relief from debilitating dry eye symptoms that traditional methods couldn’t address.
- A primary benefit is substantial reduction in discomfort, including burning, grittiness, and blurred vision, leading to improved quality of life.
- Many procedures aim for restoration of the eye’s natural physiology, rather than just symptom management, leading to more sustainable results.
- They can help prevent progression of dry eye disease and potential ocular surface damage by restoring tear film integrity.
- Reduced reliance on frequent artificial tear drops and other palliative treatments is a common and welcomed outcome.
Are there risks or considerations associated with advanced dry eye procedures?
As with any medical procedure, advanced dry eye treatments carry potential risks and considerations, though they are generally considered safe when performed by experienced specialists.
- Potential side effects can include temporary redness, swelling, discomfort, or, rarely, infection at the procedure site.
- The effectiveness of specific procedures can vary among individuals, and multiple sessions might be required for optimal results.
- Patients should discuss their full medical history and current medications with their ophthalmologist to assess individual suitability and potential contraindications.
- It’s crucial to have realistic expectations and understand that while these procedures significantly improve symptoms, they may not offer a complete “cure” for chronic conditions.