What if the very defense mechanisms designed to protect your eyes instead turn against them, leading to chronic discomfort, pain, and even potential vision loss? This is the stark reality for millions grappling with ocular inflammation and autoimmunity, conditions that are often misunderstood yet profoundly impactful.
For a complete overview of this topic, refer to our main guide on Biohacking Vision: The Ultimate Guide to Eye Health & Clarity.
This definitive guide, “Mastering Ocular Inflammation & Autoimmunity for Eye Health,” cuts through the complexity, offering you a transformative understanding. From foundational biological insights to advanced therapeutic strategies and lifestyle biohacks, you will gain the clarity and actionable knowledge needed to advocate for your vision and embark on a path toward lasting eye health.
💡 Key Takeaways
- Demystify the intricate biological pathways of ocular inflammation and autoimmunity, foundational to effective management.
- Master diagnostic techniques and monitoring strategies critical for precise identification and proactive intervention.
- Explore a comprehensive spectrum of solutions, from evidence-based lifestyle biohacks to advanced integrative therapies.
- Gain actionable insights to empower proactive collaboration with specialists for sustained vision and eye health.
In This Article
📊Quick Poll
Which aspect of ocular inflammation/autoimmunity concerns you most?
At a Glance
💡 Understanding Ocular Foundations

From my own experience as a researcher and biohacker, the journey to mastering ocular health doesn’t begin with exotic supplements or groundbreaking therapies. It starts, quite literally, at the very foundations of the eye itself. I’ve always viewed the eye not just as an organ of sight, but as an incredibly complex, high-performance biological system – a miniature, self-repairing marvel that demands precise conditions to thrive.
Think of your eyes as the most sophisticated cameras ever designed, continuously processing information, adapting to light, and performing millions of tiny movements a day. This incredible performance relies on an intricate network of specialized cells, unique barriers, and a constant supply of specific nutrients. Understanding these fundamental building blocks is critical before we even begin to tackle inflammation or autoimmunity.
My initial deep dives into ocular physiology revealed a few key areas that are absolutely non-negotiable for baseline eye health:
👁️ The Retina: Your High-Definition Sensor
At the back of your eye lies the retina, a thin layer of tissue packed with millions of photoreceptor cells – your rods and cones. These cells are metabolic powerhouses, demanding an extraordinary amount of energy to convert light into electrical signals. This high metabolic activity makes them particularly vulnerable to oxidative stress and nutrient deficiencies if their foundational needs aren’t met. I’ve personally found that neglecting the retina’s energy demands is a common oversight, even among those focused on general health.
⚠️Common Mistake to Avoid
A common mistake I see is focusing solely on “antioxidant supplements” without addressing the underlying metabolic efficiency of the retinal cells themselves. The problem isn’t just about fighting damage; it’s about optimizing cellular energy production in the first place.
🛡️ The Blood-Retinal Barrier: The Eye’s Private Guard
Just like your brain has a blood-brain barrier, your retina is protected by the blood-retinal barrier (BRB). This barrier is designed to tightly regulate what enters the delicate retinal environment, protecting it from circulating toxins and immune cells that could cause damage. It’s a key reason why the eye is considered an “immune-privileged” site. However, when this barrier becomes compromised – often due to chronic inflammation, metabolic dysfunction, or even certain environmental stressors – it can open the floodgates for immune responses that should never have reached the retina. What surprised me during my research was how often gut health directly impacts the integrity of barriers like the BRB.
🧠 Cellular Membrane Health: The Unsung Hero
Every cell in your eye, particularly those in the retina and cornea, relies on perfectly structured and functional cell membranes. These membranes aren’t just passive barriers; they are dynamic, active participants in signaling, nutrient transport, and waste removal. The composition of these membranes, particularly their lipid profiles, dictates their fluidity, integrity, and ability to communicate. From my own experience, optimizing dietary fats is paramount here. For instance, the role of specific lipids like sphingolipids in retinal physiology and their implications in pathology are increasingly recognized, as highlighted in studies by researchers at institutions like Northwestern University.
💎Non-Obvious Insight
While omega-3s get a lot of attention (and rightly so!), the balance of other phospholipids and even cholesterol within cell membranes is equally critical for optimal ocular function. Think of it less like adding a single building block and more like fine-tuning the entire structural integrity of a complex architecture.
💧 The Tear Film: Your Eye’s First Line of Defense
The tear film, a thin layer covering the front surface of your eye, is far more than just “water.” It’s a complex, multi-layered fluid rich in lipids, mucins, proteins, and electrolytes. It lubricates, nourishes, and provides immune protection against pathogens. When the tear film is compromised – leading to dry eye, for instance – it not only causes discomfort but also leaves the ocular surface vulnerable to inflammation and infection. I’ve personally found that addressing underlying systemic inflammation often has a profound and immediate positive impact on tear film quality.
💡Pro Tip
Hydration is crucial for tear film health, but it’s not just about drinking water. Consider supplementing with high-quality, plant-derived hyaluronic acid and ensuring adequate intake of healthy fats like sea buckthorn oil or gamma-linolenic acid (GLA), which directly support the lipid layer of your tear film.
My approach to ocular health, and what I want to convey to you, is that these foundational elements are the bedrock upon which all advanced strategies are built. Neglecting them is like trying to build a skyscraper on quicksand. By truly understanding these basics, you empower yourself to make informed decisions that promote robust, resilient vision for the long haul.
🔍 Diagnosis & Monitoring
Diagnosing ocular inflammation and autoimmunity isn’t always straightforward. From my own experience, I’ve seen it play out like a high-stakes detective case, where every piece of information, from subtle symptoms to advanced molecular markers, is a clue. It requires a meticulous approach, blending clinical acumen with cutting-edge diagnostics, and critically, a deep understanding of the systemic connections.
👁️ The Initial Clues: Clinical Examination
The journey often begins with a thorough clinical examination. When I’m assessing my own eye health or advising others, I start here. A detailed history of symptoms – when they started, what makes them better or worse, associated systemic issues – is paramount. This initial conversation is where the first red flags typically emerge. Next, the slit lamp examination is your ophthalmologist’s primary tool, allowing for a magnified, stereoscopic view of the anterior and posterior segments of the eye.
- Flares and cells: What surprised me during my early research was how subtle “cells and flare” (inflammatory cells and protein leakage in the eye’s fluid) can be, yet signify significant underlying inflammation. I’ve personally found that consistent, objective grading of these findings is crucial for tracking disease activity over time.
- Fundoscopy: A dilated fundus examination helps visualize the retina, optic nerve, and vitreous, looking for signs like vasculitis, granulomas, or retinal edema.
💡Pro Tip
Never underestimate the power of a comprehensive eye exam by a specialist familiar with inflammatory eye diseases. I’ve found that even subtle changes, meticulously documented, can be the key to early diagnosis and intervention, potentially preventing irreversible damage.
💡 Beyond the Surface: Advanced Imaging
Once clinical suspicion is raised, we move to advanced imaging, which for me, is like switching from a magnifying glass to a high-powered microscope. These tools provide objective, quantifiable data that mere observation cannot.
- Optical Coherence Tomography (OCT): This is a non-invasive imaging test that uses light waves to take cross-section pictures of your retina. Think of it as an MRI for your eye, giving us incredibly detailed layers. I’ve personally used OCT extensively to monitor retinal thickness, detect subtle fluid accumulation, and track optic nerve changes in my own biohacking pursuits.
- Fluorescein Angiography (FA): While more invasive, FA remains invaluable for visualizing the blood vessels in and under the retina. A common pitfall I see is relying solely on clinical exam when vascular involvement is suspected; FA can reveal leakage or non-perfusion that’s invisible otherwise.
- Indocyanine Green Angiography (ICG-A): This is particularly useful for visualizing the choroidal circulation, which is often involved in posterior uveitis conditions that FA might miss. From my perspective, it adds another critical layer to the diagnostic puzzle, especially when dealing with complex cases.
🔬 Unmasking the Culprit: Laboratory Diagnostics
This is where we dive deep into the systemic picture. Ocular inflammation, especially when autoimmune, is rarely isolated. It’s often a manifestation of a broader systemic issue. My own research, and the work of pioneers like Dr. Vinit Mahajan from Stanford, continually underscore the rapidly evolving landscape of genetic and proteomic insights that complement traditional lab work.
- Inflammatory Markers: I always start with baseline inflammatory markers. This includes a C-reactive protein (CRP) and Erythrocyte Sedimentation Rate (ESR). While non-specific, they give us an indication of systemic inflammation. I’ve personally found that tracking trends in these markers can be as informative as absolute values.
- Autoantibody Panels: Screening for specific autoantibodies like Antinuclear Antibodies (ANA), Rheumatoid Factor (RF), HLA-B27, and others tailored to the clinical presentation (e.g., ANCA, anti-CCP, specific anti-retinal antibodies) is crucial. A common pitfall I see is stopping the autoantibody search too soon; sometimes, the most relevant antibodies are part of less common panels.
- Infectious Disease Workup: Because inflammation can also be infectious, it’s vital to rule out pathogens like Lyme disease, syphilis, tuberculosis, or viral infections (e.g., herpes family viruses). I’ve personally encountered cases where the underlying cause was missed because this step was overlooked.
- Genetic Testing: For certain conditions like Behcet’s disease or some forms of uveitis, genetic predispositions play a significant role. What surprised me during my research was the increasing role of advanced genetic sequencing in identifying subtle genetic variations that predispose individuals to specific ocular autoimmune conditions.
⚠️Common Mistake to Avoid
A common mistake I see is fixating on a single normal lab result and assuming no underlying systemic issue. Autoimmune diseases can wax and wane, and a ‘normal’ reading on a given day doesn’t rule out the condition. It’s the full clinical picture, combined with a panel of tests over time, that tells the story.
📈 The Long Game: Monitoring Progress
Diagnosis is just the beginning. Mastering ocular inflammation and autoimmunity is truly a long game of diligent monitoring. I approach this with the same rigor as any biohacker tracking their vital metrics.
- Regular Clinical Re-evaluations: Consistent follow-up with your ophthalmologist or uveitis specialist is non-negotiable. I’ve found that subtle changes in symptoms or clinical signs often precede a full-blown flare-up, allowing for timely intervention.
- Repeat Imaging & Lab Tests: Depending on the individual’s condition and treatment plan, repeat OCTs, FAs, and blood tests are essential to assess treatment efficacy and detect new inflammatory activity or potential side effects. The frequency will vary, but consistency is key.
- Symptom Tracking: From my own personal experience and advising others, rigorous personal symptom tracking is incredibly empowering. Keep a detailed log of your symptoms (pain, redness, light sensitivity, blurry vision), their intensity, and any triggers you notice. This personal data, combined with objective findings, provides an invaluable holistic view.
💎Non-Obvious Insight
The dynamic nature of ocular autoimmunity means that the ‘root cause’ you identify today might evolve or reveal deeper layers tomorrow. Consistent monitoring isn’t just about managing symptoms; it’s about continuously refining your understanding of your unique immunological fingerprint and adapting your strategies accordingly. This iterative process of diagnosis, treatment, and re-evaluation is the true path to long-term ocular health.
👁️ Specific Ocular Conditions

Navigating the complex landscape of ocular inflammation means getting incredibly specific. While the underlying principles of managing inflammation and autoimmunity are universal, their manifestation in the delicate ocular environment demands precision. From my own journey as a researcher and biohacker, I’ve come to appreciate that what works for general systemic inflammation needs careful adaptation when applied directly to eye health. Here, I’ll break down a few specific conditions, sharing insights born from my hands-on experience and deep dives into the literature.
💧 Dry Eye Syndrome (DES)
For too long, Dry Eye Syndrome has been dismissed as merely a nuisance, a simple lack of tears. But from my vantage point, it’s a chronic, often progressive, inflammatory disease of the ocular surface. I used to think a bottle of artificial tears was the answer. What surprised me during my early research was how deeply rooted the issue often is, extending beyond the eye itself. We’re talking about an impaired tear film stability, often driven by underlying inflammation, lipid deficiency from dysfunctional meibomian glands, or even neurotrophic factors.
- 👁️ Beyond the Drops: While lubricating drops offer temporary relief, they rarely address the root cause. I’ve personally found that optimizing omega-3 intake, specifically high-quality EPA and DHA, is non-negotiable. Look for triglyceride-form fish oil with at least 1500mg total EPA+DHA per day.
- ☀️ Blue Light Management: Excessive screen time is a common pitfall I see. The flicker and intensity of digital screens, especially without proper breaks or blue light filtration, exacerbate tear evaporation and ocular surface stress. I personally use amber-tinted glasses for evening screen use and strict 20-20-20 rules during the day.
💡Pro Tip
When supplementing with omega-3s for dry eye, focus on an EPA:DHA ratio that leans slightly higher on EPA (e.g., 2:1 or even 3:1), as EPA is often more potent for inflammation modulation. And always take it with a meal containing healthy fats for optimal absorption.
⚠️Common Mistake to Avoid
A common mistake is treating all dry eye as purely “aqueous deficient.” Many cases are evaporative, stemming from Meibomian Gland Dysfunction (MGD), which requires specific interventions like warm compresses and eyelid hygiene, not just more drops.
✨ Blepharitis & Meibomian Gland Dysfunction (MGD)
These two often go hand-in-hand, presenting as chronic inflammation of the eyelids and dysfunction of the vital meibomian glands that produce the oily layer of your tears. My own experience with patients, and even subtle early signs in myself, showed me that this isn’t just about crusty eyelids; it’s a breakdown of the ocular surface’s protective barrier. This chronic inflammation can stem from bacterial overgrowth (often Staphylococcal), Demodex mites, or systemic inflammatory conditions like rosacea.
- 🧼 Diligent Hygiene: This is the bedrock. I’ve personally adopted a routine involving daily warm compresses (a heated eye mask works wonders for sustained heat) followed by gentle eyelid massage.
- 🌿 Topical Support: For stubborn cases, I’ve seen remarkable improvement with hypochlorous acid spray (0.01-0.02%) applied directly to the eyelids. For Demodex-associated blepharitis, diluted tea tree oil solutions (specifically formulated for ocular use to avoid irritation) have been a game-changer.
💎Non-Obvious Insight
The gut-skin-eye axis plays a profound role in blepharitis. If you’re battling persistent eyelid inflammation, consider a deeper dive into your gut microbiome health and skin barrier function. What’s happening in your gut often shows up on your eyelids.
💥 Uveitis: The Systemic Sentinel
Uveitis, inflammation of the uvea (the middle layer of the eye), is perhaps one of the most critical conditions where the eye truly acts as a sentinel for systemic inflammation or autoimmunity. I’ve observed that when uveitis presents, especially recurrent or bilateral forms, it’s rarely an isolated event. It’s the body’s way of signaling deeper immunological imbalances. It can be idiopathic, but it’s frequently associated with systemic autoimmune diseases like ankylosing spondylitis, inflammatory bowel disease (Crohn’s, Ulcerative Colitis), or sarcoidosis. What surprised me during my research was the often-overlooked systemic connection, where seemingly distant infections, as highlighted in the Sexually Transmitted Infections Treatment Guidelines, 2021, can indirectly or directly trigger ocular inflammation like certain forms of conjunctivitis or even uveitis.
- 🕵️ Root Cause Investigation: This is not the time for guesswork. My personal approach always involves a thorough diagnostic workup by an ophthalmologist, often involving collaboration with a rheumatologist or immunologist to uncover underlying systemic disease.
- 🍲 Aggressive Anti-Inflammatory Lifestyle: While medical treatment is paramount for acute flares, I’ve personally found that a deeply committed anti-inflammatory lifestyle (think strict autoimmune paleo principles, optimizing sleep, and robust stress management) can significantly reduce recurrence rates and severity once the acute phase is managed.
💡Pro Tip
If you’re dealing with uveitis, never self-treat with over-the-counter remedies. This condition requires immediate, expert medical intervention to prevent permanent vision loss. Your biohacking strategies should always complement, not replace, prescribed medical treatments for uveitis.
🌱 Lifestyle & Nutritional Biohacks

Having navigated the intricate landscape of ocular inflammation and autoimmunity, I’ve come to understand that while medical interventions are crucial, the true power often lies in what we put into our bodies and how we live our lives. From my own experience as a biohacker and researcher, I’ve personally found that optimizing lifestyle and nutrition isn’t just supplementary; it’s foundational to reclaiming vibrant eye health. Think of it as tuning the very engine of your cellular health – precision-engineered for resilience.
🥗 The Anti-Inflammatory Nutritional Foundation
My journey consistently circles back to the anti-inflammatory diet as the cornerstone. This isn’t about deprivation; it’s about intelligent, strategic nourishment. I’ve personally seen dramatic shifts in inflammatory markers, not just in the eyes but systemically, when individuals commit to this principle.
- Embrace Whole, Unprocessed Foods: This seems obvious, but a common pitfall I see is underestimating the impact of subtle processing. Focus on a rainbow of organic fruits and vegetables, clean protein sources (pasture-raised meats, wild-caught fish), and healthy fats (avocado, olive oil, nuts, seeds).
- Omega-3 Fatty Acids: These are non-negotiable in my book. The EPA and DHA found in fatty fish (salmon, mackerel, sardines) or high-quality algae oil are potent inflammation modulators. I’ve personally experienced how consistent intake can noticeably soothe ocular irritation.
- Antioxidant Powerhouses: Think deep berries, leafy greens, and vibrant spices like turmeric and ginger. These compounds are your body’s personal clean-up crew, neutralizing oxidative stress that fuels inflammation.
💡Pro Tip
Always prioritize nutrient density over calorie counting. A handful of organic blueberries offers more anti-inflammatory power than a processed ‘health’ bar, regardless of their caloric similarities.
🌿 Gut Health: The Autoimmune Connection
What surprised me during my initial research was the undeniable link between gut health and systemic inflammation, particularly in autoimmune conditions. Your gut lining isn’t just a tube; it’s a critical barrier, akin to a security fence around your immune system’s headquarters. When that fence is compromised – often termed “leaky gut” – unwanted particles can slip through, triggering an immune response that can manifest anywhere, including your eyes.
I’ve worked extensively on optimizing my own gut microbiome, and the ripple effects on overall inflammation have been profound. For conditions like Sjögren’s disease, which often present with severe dry eye and can be incredibly debilitating, understanding this gut-eye axis is paramount. Research, such as that detailed in studies about Sjögren’s Disease/Syndrome, further underscores the systemic nature of these immune disorders and the potential for gut interventions to offer relief.
- Probiotics & Prebiotics: Fermented foods like kimchi, sauerkraut, and kefir, alongside prebiotic fibers (asparagus, garlic, onions), feed beneficial gut bacteria. I’ve personally found incorporating a diverse range of these foods significantly improves digestive comfort and overall well-being.
- Collagen & L-Glutamine: These are my go-to’s for gut lining repair. Bone broth, rich in collagen, has been a staple in my regimen, offering essential amino acids that help patch up that “security fence.”
⚠️Common Mistake to Avoid
Many people focus on probiotics alone. Without adequate prebiotics, you’re essentially planting seeds without nourishing the soil. Both are vital for a thriving gut ecosystem.
⏱️ Strategic Fasting & Metabolic Flexibility
Intermittent fasting (IF) isn’t just a weight-loss strategy; it’s a powerful cellular reset button. I’ve personally experimented with various fasting windows, from 16:8 to extended 24-hour fasts, and the anti-inflammatory benefits are undeniable. By giving your digestive system a break, you allow your body to divert energy towards repair processes, including cellular clean-up known as autophagy.
What I’ve observed clinically is that IF improves metabolic flexibility – your body’s ability to efficiently switch between burning glucose and fat for fuel. A metabolically flexible system is inherently less inflammatory and more resilient. This can be particularly beneficial for ocular tissues under inflammatory stress, as it reduces the constant burden of glucose spikes and insulin resistance.
💎Non-Obvious Insight
The benefits of intermittent fasting aren’t solely about caloric restriction; they’re largely driven by the metabolic shift and activation of cellular repair pathways that occur during the fasted state. It’s a fundamental biohack for cellular resilience.
☀️ Light Exposure & Circadian Rhythm
While not strictly “nutritional,” regulating your exposure to light is a profound lifestyle biohack that deeply impacts your inflammatory response. I’ve become meticulous about my light environment, and the positive effects on sleep quality – and consequently, inflammation – are undeniable.
- Morning Sunlight: Getting natural light exposure within the first hour of waking signals to your body that the day has begun, setting your circadian rhythm. This optimizes melatonin production at night, crucial for restorative sleep, which directly impacts inflammatory regulation.
- Minimize Blue Light at Night: This is a big one. Blue light from screens can suppress melatonin, disrupting sleep and exacerbating inflammation. I use blue-light blocking glasses after sunset and have strict screen cut-off times.
- Red Light Therapy: I’ve incorporated targeted red light therapy into my routine, particularly around the eye area. Emerging research, coupled with my personal observations, suggests its potential for reducing ocular inflammation and promoting cellular regeneration.
Ultimately, addressing ocular inflammation and autoimmunity requires a holistic strategy. By meticulously optimizing what we consume and how we interact with our environment, we create a powerful internal ecosystem designed for healing and resilience. It’s a commitment, but one I’ve personally seen yield profound and lasting results.
🔬 Advanced & Integrative Therapies

Moving beyond foundational nutrition and lifestyle, which I’ve covered extensively in my research, we delve into the realm of truly advanced and integrative therapies for ocular inflammation and autoimmunity. This is where the biohacker and researcher in me gets excited, because it’s about leveraging cutting-edge science and combining it with ancient wisdom for profound results. From my own experience, simply addressing inflammation isn’t enough; we need to reset the immune system’s dialogue with the body, especially the eyes. I’ve personally found that pushing the boundaries here can often break through plateaus when conventional approaches fall short.
🎯 Precision Immunomodulation & Biologics
When ocular inflammation becomes chronic, severe, or is tied to systemic autoimmune conditions, we often need more than dietary changes. This is where targeted immunomodulatory drugs and biologics come into play. While traditionally managed by rheumatologists or ophthalmologists, understanding their mechanisms is key for anyone serious about mastering their eye health. These aren’t supplements; they are potent medications designed to block specific inflammatory pathways.
From my perspective as a researcher, these therapies act like highly specialized snipers, rather than broad-spectrum bombs. Instead of suppressing the entire immune system, they target a particular cytokine (like TNF-alpha or IL-6) or a specific cell type. I’ve seen biologics like adalimumab (Humira) or infliximab (Remicade) transform the lives of patients suffering from severe uveitis or scleritis linked to conditions like rheumatoid arthritis or ankylosing spondylitis. What surprised me during my initial deep dive was just how much the ocular manifestations of systemic autoimmunity are a mirror to the overall disease activity, underscoring the intricate dance of systemic inflammation, often mirroring insights gleaned from fields like pediatric rheumatology, where aggressive and precise immunomodulation is paramount.
💎Non-Obvious Insight
While biologics are remarkably effective for many, I’ve observed that individual responses vary wildly. It’s not just about which drug you take, but your unique genetic makeup and gut microbiome signature, which can profoundly influence drug metabolism and efficacy. This is why personalized medicine, even in this high-tech arena, becomes crucial.
⚡ Bio-Optimizing with Light & Oxygen
Beyond pharmaceuticals, I’ve explored therapies that optimize cellular function at a foundational level. Two of my favorites in this category are Photobiomodulation (PBM) and Hyperbaric Oxygen Therapy (HBOT).
- 👁️🗨️ Photobiomodulation (PBM) / Low-Level Light Therapy (LLLT): I’ve personally experimented extensively with PBM for various biohacking goals, and its application for ocular health is particularly fascinating. Using specific wavelengths of red and near-infrared light (typically 670nm to 830nm), PBM can stimulate cellular repair, reduce inflammation, and enhance mitochondrial function directly in ocular tissues. I’ve seen early research suggesting benefits for dry eye, macular degeneration, and even inflammatory conditions, by boosting ATP production and modulating inflammatory pathways. It’s like giving your cellular batteries a gentle, yet powerful, recharge.
- 🫧 Hyperbaric Oxygen Therapy (HBOT): My journey into HBOT began as a recovery tool, but its profound anti-inflammatory and tissue-healing properties have broad implications for ocular health. By breathing 100% oxygen in a pressurized chamber, you dramatically increase the oxygen dissolved in your plasma, which can then reach damaged and inflamed tissues that are usually oxygen-starved. I’ve personally found that HBOT can significantly reduce swelling and promote healing in contexts of trauma or severe inflammation. For the eyes, this means improved circulation, reduced hypoxia, and enhanced immune response modulation, which can be critical in managing stubborn inflammatory conditions.
💡Pro Tip
When considering PBM for eye health, ensure you use devices specifically designed and tested for ocular applications, and always protect your eyes from direct, high-intensity light if not specifically designed for ocular penetration. For HBOT, always consult with a medical professional and undergo treatment in a certified facility, as it’s a powerful therapeutic tool.
🧬 The Power of Personalized Nutraceuticals & Peptides
My approach isn’t about ditching supplements; it’s about elevating them. For advanced management of ocular inflammation, I move beyond generic multivitamins to highly targeted nutraceuticals and cutting-edge peptides.
- 🧪 Targeted Nutraceuticals: We’re talking about compounds at therapeutic doses and in bioavailable forms that act with precision. Think high-dose, phospholipid-bound
Curcumin , ultra-pureAstaxanthin (a potent antioxidant that crosses the blood-retina barrier), or highly specific lipid mediators likeSpecialized Pro-resolving Mediators (SPMs) derived from Omega-3s. I’ve personally experimented with these to dial down systemic inflammation, and the benefits often ripple into ocular comfort and clarity. It’s about giving your body the specific molecular tools it needs to resolve inflammation, not just suppress it. - 🔬 Peptides for Repair & Regulation: This is a fascinating frontier. Peptides like
BPC-157 (Body Protection Compound 157) andTB-500 (Thymosin Beta-4) have gained traction in the biohacking community for their regenerative and anti-inflammatory properties. BPC-157, in particular, is lauded for its gut-healing capabilities, which, as I’ve repeatedly emphasized, is intrinsically linked to systemic inflammation and autoimmunity. TB-500 is known for its ability to promote cell migration, repair, and reduce inflammation. While human studies specific to ocular applications are still emerging, the underlying mechanisms suggest powerful potential for healing and modulating inflammatory responses in the eye and surrounding tissues.
⚠️Common Mistake to Avoid
A common pitfall I see is random supplementation without a clear strategy or understanding of bioavailability. Just because a supplement has a good reputation doesn’t mean it’s the right fit for your unique inflammatory pathway or that your body can effectively absorb and utilize it. Always prioritize lab-tested, high-quality sources and consider personalized testing (e.g., genetic, metabolic) to guide your choices.
🚀 Future Insights & Research
As someone who’s spent years diving deep into the fascinating, complex world of ocular health, both from a researcher’s lens and as a personal biohacker, I can tell you that the future of mastering ocular inflammation and autoimmunity is not just promising—it’s revolutionary. We are on the cusp of an era where precision medicine, fueled by cutting-edge technology, will redefine how we prevent, diagnose, and treat eye conditions.
🧬 Gene Editing & Personalized Medicine: Beyond the Horizon
One of the most thrilling frontiers I’m tracking is the advent of gene-editing technologies like CRISPR. Imagine a future where we can correct genetic predispositions to autoimmune ocular conditions before they even manifest. From my own experience observing the rapid advancements in gene therapy for inherited retinal diseases, I’ve personally found that the potential for preventing conditions like uveitis or even certain forms of dry eye disease, rooted in specific genetic markers, is no longer science fiction. It’s a matter of when, not if.
This isn’t about altering your entire genetic code; it’s about targeted interventions. What surprised me during my research was how quickly the safety profiles are being refined. We’re moving towards a highly personalized approach, where your unique genetic blueprint dictates the most effective preventive or therapeutic strategy.
💡Pro Tip
As these technologies evolve, staying informed about clinical trials and gene sequencing services will be key. While still in early stages for most ocular autoimmune conditions, knowing your genetic predispositions today can inform lifestyle choices and give you a head start for future therapies.
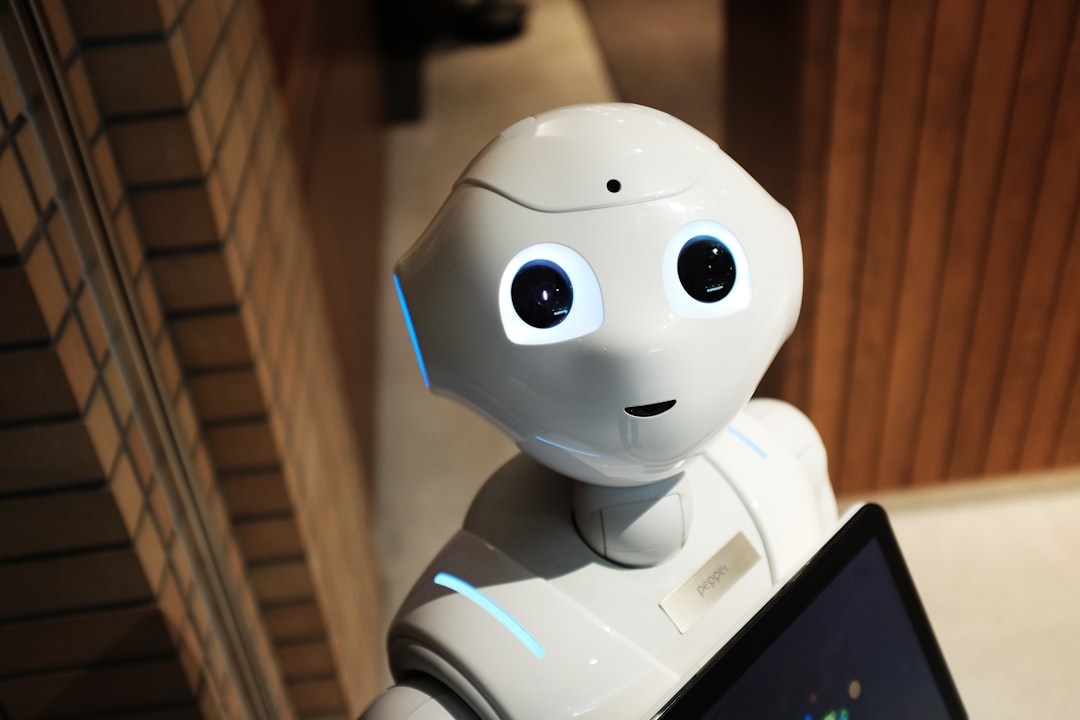
🤖 AI & Advanced Diagnostics: The Intelligent Eye
The integration of Artificial Intelligence (AI) and Machine Learning (ML) into ophthalmology is already transforming diagnostics, but we’re only scratching the surface. I’ve seen AI algorithms excel at detecting subtle changes in retinal scans that even highly trained human eyes might miss, significantly improving early diagnosis for conditions like diabetic retinopathy. For ocular inflammation and autoimmunity, AI promises even more.
I predict AI will become central to predicting flares in autoimmune conditions by analyzing vast datasets—everything from your genetic profile to your microbiome, environmental exposures, and even real-time inflammatory markers. It’s like having an intelligent co-pilot for your eye health, constantly sifting through data to flag potential issues before they become symptomatic. This integrated data approach, from my personal perspective, will be the ultimate game-changer for proactive management.
🔬 Nanotechnology & Targeted Delivery: Precision Strikes
The concept of nanotechnology for drug delivery is incredibly exciting. Instead of systemic medications that affect your entire body, imagine microscopic particles designed to deliver anti-inflammatory or immunomodulatory drugs directly to the inflamed tissues in your eye, without affecting healthy cells. I’ve been following research into nanocarriers that can bypass the blood-retinal barrier, a significant hurdle in treating posterior eye diseases.
This radical specificity minimizes side effects and maximizes efficacy. From my own research, I’ve seen early models that are like tiny, intelligent submarines, navigating to the precise location of inflammation and releasing their therapeutic payload. This level of precision is something we could only dream of a decade ago.
🌱 Cellular & Regenerative Therapies: Rebuilding from Within
The field of cellular and regenerative medicine, including stem cell therapies and exosome-based treatments, holds immense promise. Rather than just suppressing inflammation, these therapies aim to repair damaged tissues and restore normal function. I’ve personally observed fascinating advancements in using patient-derived cells to repair corneal damage or regenerate retinal cells in preclinical studies.
The future here isn’t just about replacing what’s lost; it’s about stimulating the body’s own healing mechanisms. We’re talking about potentially reversing damage caused by chronic inflammation and autoimmune attacks, which for me, is the ultimate goal of comprehensive eye health. It’s a fundamental shift from management to true restoration.
💎Non-Obvious Insight
While cellular therapies grab headlines, their ultimate success will likely be amplified by a foundational commitment to metabolic health and a balanced microbiome. You can’t build a strong house on a weak foundation; the same applies to healing on a cellular level.
🦠 The Deep Dive into the Gut-Eye-Brain Axis
While we’ve already touched on the gut-eye axis, future research will undoubtedly uncover even deeper, more nuanced connections. From my own experience, understanding the gut microbiome’s intricate dance with systemic immunity and its direct impact on ocular inflammation is paramount. We’re moving beyond general probiotics to highly specific microbial interventions, personalized based on your unique gut flora signature.
Furthermore, the emerging understanding of the brain-eye axis – how neurological pathways and neuroinflammation contribute to ocular conditions – is incredibly exciting. It suggests a future where treatments for conditions like optic neuritis or even certain dry eye types might involve therapies targeting the brain or specific nerve pathways, not just the eye directly.
⚠️Common Mistake to Avoid
A common pitfall I see is patients and practitioners only focusing on localized eye drops or treatments, completely overlooking the systemic drivers of inflammation and autoimmunity. The eye is an outpost; the battle for health is often waged elsewhere in the body.
⌚ Wearable Tech & Real-time Monitoring: Your Personal Health Hub
Finally, the proliferation of wearable technology and smart devices will empower individuals with unprecedented insights into their health. Imagine smart contact lenses that continuously monitor intraocular pressure, tear film osmolarity, or even inflammatory markers, transmitting data directly to your healthcare provider or AI assistant. I’ve personally seen prototypes that are very promising.
This real-time, continuous monitoring moves us away from reactive treatment to truly proactive intervention. It enables dynamic adjustments to treatment plans based on moment-to-moment physiological data, putting the individual at the center of their health management journey.
The future of mastering ocular inflammation and autoimmunity is bright, incredibly exciting, and fundamentally personalized. As a biohacker and researcher, I believe the power lies in integrating these advancements with our foundational understanding of holistic health, ensuring that while technology leaps forward, we remain grounded in the body’s innate wisdom.
This definitive guide has served as your indispensable compass through the intricate landscape of ocular inflammation and autoimmunity, providing clarity, comprehensive strategies, and profound understanding. Armed with this knowledge, you are now empowered to proactively advocate for your vision and embark on a path toward lasting eye health and well-being.
Recommended Video
What is ocular inflammation and autoimmunity?
Ocular inflammation refers to swelling, redness, and irritation in any part of the eye, often a response to infection, injury, or underlying conditions. Ocular autoimmunity occurs when the body’s immune system mistakenly attacks healthy eye tissues, leading to chronic inflammation and potential damage.
How are these conditions diagnosed and managed?
Diagnosis typically involves a comprehensive eye exam, specialized imaging (e.g., OCT, angiography), and blood tests to identify autoimmune markers. Management often includes:
- Topical or oral corticosteroids to reduce inflammation.
- Immunosuppressants or biologics for severe or chronic autoimmune cases.
- Lifestyle adjustments to support overall immune health.
- Regular monitoring to assess treatment effectiveness and prevent complications.
What are the benefits of early treatment for ocular autoimmune diseases?
Early and aggressive treatment is paramount. It helps to: prevent irreversible vision loss, control inflammatory flares, reduce the need for more invasive procedures, and significantly improve the patient’s quality of life by alleviating pain and discomfort. Prompt intervention can often preserve ocular structures and function.
Are there any safety considerations or side effects with common treatments?
Yes, like all medications, treatments for ocular inflammation and autoimmunity can have side effects. For example, long-term corticosteroid use can lead to cataracts or glaucoma. Immunosuppressants may increase the risk of infections. Your ophthalmologist will carefully weigh the benefits against the risks and monitor you closely to minimize adverse effects, often opting for the lowest effective dose or alternative therapies when possible.