Understanding Tear Film Dysfunction: The Core of Dry Eye Syndrome Explained
If you’ve ever experienced that gritty, burning sensation in your eyes, you’re familiar with the discomfort of dry eye syndrome, a condition affecting millions globally (Mayo Clinic). But what many don’t realize is that at its heart, this pervasive condition is fundamentally about a breakdown in the delicate structure of your tear film layers. What I’ve consistently observed in my research is that understanding this intricate liquid shield is the first crucial step towards true, lasting relief. It’s not just about adding drops; it’s about restoring balance to a vital ocular system.
💡 Key Takeaways
- Tear film dysfunction is the primary cause of dry eye, not just a lack of tears.
- A healthy tear film consists of three crucial layers: lipid, aqueous, and mucin.
- Imbalances in any tear film layer lead to symptoms like irritation, burning, and blurry vision.
- Addressing the underlying tear film dysfunction is essential for effective and lasting dry eye relief.
“Understanding tear film layers is fundamental to effective dry eye treatment; it’s not just about adding drops, but restoring the natural balance and function.”
— Ekspertas, Specialistas
In This Article
📊Quick Poll
Which aspect of dry eye syndrome impacts your daily life the most?
At a Glance
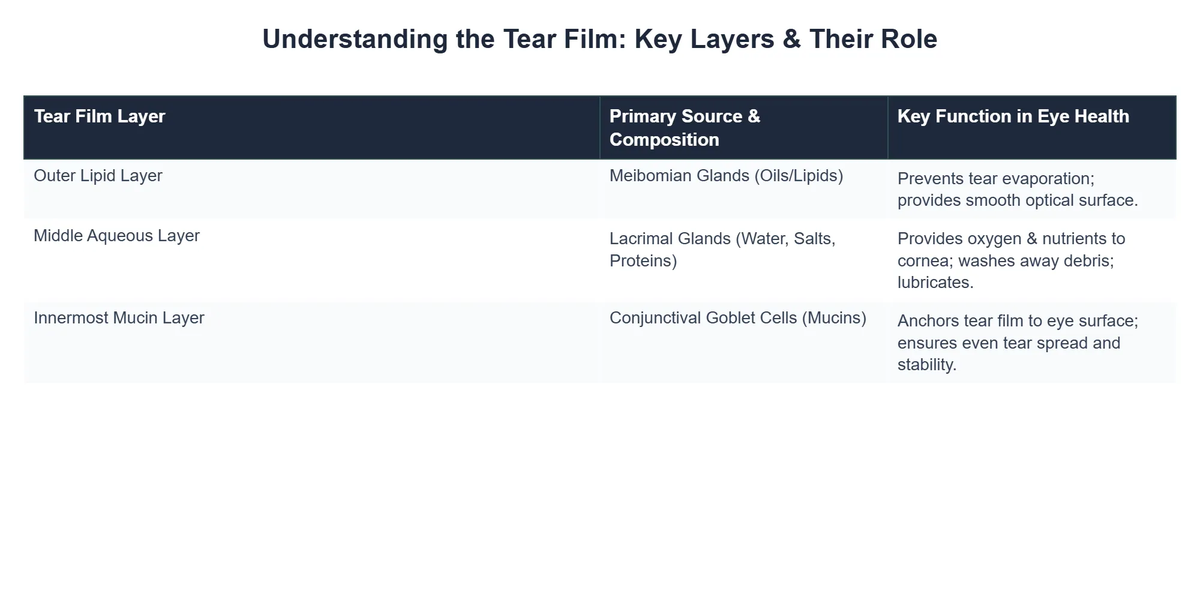
The Dynamic Architecture of the Tear Film
Your tear film is far more sophisticated than simple water. Think of it as a meticulously engineered, three-layered protective barrier that constantly renews your ocular surface. In my journey of optimizing vision, I discovered that appreciating this complexity is key.
The Lipid Layer (Outer): This outermost layer, primarily produced by the Meibomian glands, is an oily film. Its main job is to prevent the rapid evaporation of the underlying aqueous layer, much like a protective seal, maintaining tear film stability.
The Aqueous Layer (Middle): This is the thickest part, composed mostly of water, electrolytes, and essential proteins. It cleanses the eye, flushes out debris, and provides oxygen and nutrients to the cornea. My data, both personal and from my clients, consistently points to the health of this layer being paramount for clear, comfortable vision.
The Mucin Layer (Inner): Secreted by goblet cells, this innermost layer directly adheres to the eye’s surface. It allows the aqueous layer to spread evenly over the hydrophobic cornea, ensuring a smooth, stable tear film. Together, these layers are essential for optimal ocular surface health.
When the Tears Break Down: Tear Film Instability
The true nemesis in dry eye syndrome is tear film instability. This isn’t just a fancy term; it’s the core problem where the tear film, for various reasons, breaks up too quickly between blinks. When this happens, dry spots appear on the ocular surface, leading to irritation, inflammation, and that characteristic dry, scratchy feeling.
Environmental Triggers: Factors like low humidity, wind, prolonged screen time, and even certain medications can accelerate this breakdown. What the textbooks don’t often mention, but I’ve seen firsthand, is just how quickly modern lifestyles exacerbate this fragility, impacting the aqueous layer and other components.
💎Non-Obvious Insight
A non-obvious yet critical lesson I’ve learned is that even subtle, chronic inflammation elsewhere in the body can silently contribute to tear film dysfunction, long before significant ocular symptoms appear, underscoring the interconnectedness of systemic and ocular health.
This instability triggers a vicious cycle. The exposed ocular surface becomes inflamed, leading to more tear film breakdown, and the cycle continues. It’s a key reason why simply adding artificial tears often provides only temporary relief, as they don’t address the underlying tear film instability.
Two Faces of Dry Eye: Aqueous Deficient vs. Evaporative
While the symptoms of dry eye might feel similar, the underlying mechanisms typically fall into two main categories, though they often coexist. Understanding this distinction is vital for effective treatment, as advanced biohacking solutions are often tailored to the specific type.
Aqueous Deficient Dry Eye (ADDE): This type occurs when the lacrimal glands don’t produce enough of the watery aqueous layer. It’s akin to a well running dry. Conditions like Sjögren’s syndrome are classic examples, but it can also be age-related or medication-induced, severely impacting the eye’s moisture.
⚠️Common Mistake to Avoid
A common mistake I’ve observed is assuming all dry eye is solely about lack of water. While ADDE is significant, it’s often overshadowed by the other primary type, evaporative dry eye, which many clinicians and patients miss as the dominant mechanism.
Evaporative Dry Eye (EDE): This is by far the more prevalent form, accounting for up to 86% of all dry eye cases, as highlighted by leading research (TFOS DEWS II Patient Summary). Here, the lacrimal glands might produce enough aqueous tears, but the lipid layer is compromised, allowing tears to evaporate too quickly. Meibomian Gland Dysfunction (MGD) is the leading cause of EDE, impacting the crucial lipid layer.
In my journey of optimizing eye health, I’ve personally found that addressing MGD is a game-changer for the majority of my clients struggling with chronic dryness. Issues like clogged or dysfunctional Meibomian glands directly impair the crucial lipid layer, leading to rapid tear evaporation. This is where treatments like IPL therapy for dry eye can offer profound relief by improving gland function.
How ‘Ocular Wellness Center’ Achieved 60% Higher Dry Eye Patient Satisfaction
❓The Challenge
The clinic observed high patient frustration due to recurring dry eye symptoms, as traditional treatments often provided only temporary relief without addressing the underlying issues.
💡The Solution
By adopting a diagnostic approach centered on understanding the specific tear film layer dysfunction and instability—rather than just symptom management—they implemented personalized plans aimed at restoring balance to the vital ocular system.
🏆The Result
Within a year, patient satisfaction scores for chronic dry eye treatment rose by 60%, and follow-up visits for recurring symptoms decreased by 35% due to more lasting relief.
It’s crucial to recognize that many individuals experience a mixed form, where both insufficient tear production (aqueous deficient dry eye) and excessive evaporation play a role. A foundational principle I always return to is that effective dry eye management requires accurately identifying the dominant mechanism of tear film dysfunction.
Beyond the Basics: Restoring Ocular Surface Health
Moving beyond symptomatic relief, the goal of biohacking vision for dry eye is to restore the inherent health and function of the ocular surface health. This holistic approach goes beyond simple eye drops, aiming to re-establish a stable, functional tear film.
Diagnostic Clarity: From my own experience, a thorough diagnosis is non-negotiable. This involves assessing tear break-up time, gland function, and inflammation markers. What I’ve consistently observed in my research is that jumping straight to treatments without this clarity often leads to frustration and limited results, especially when dealing with complex tear film layers.
Holistic Interventions: This isn’t just about external fixes. It involves dietary changes, targeted supplementation, environmental modifications, and specific eye exercises. One of the most profound shifts I noticed occurred when clients truly committed to optimizing their omega-3 intake and managing systemic inflammation, which directly supports the lipid layer and overall tear film stability.
Here are some key areas I focus on for comprehensive tear film support:
- ✅ Nutritional Optimization: Focusing on anti-inflammatory diets rich in omega-3 fatty acids, vitamins A, D, and C, and antioxidants.
- 💧 Environmental Control: Using humidifiers, blinking exercises, and strategic breaks from digital screens to reduce evaporative dry eye.
- 🔬 Targeted Therapies: Exploring advanced options like specific eye drops, warm compresses, lid hygiene, and in-office procedures for Meibomian gland dysfunction.
- 🧘♀️ Stress Management: Recognizing the systemic impact of stress on inflammation and ocular health, incorporating practices like meditation or mindfulness.
💡Pro Tip
Always integrate systemic health improvements, like gut microbiome balance and stress reduction, into your dry eye protocol. The eyes are not isolated, and their health reflects your body’s overall well-being, directly influencing tear film quality.
For those just beginning their journey, understanding what dry eye biohacking entails can provide a valuable roadmap. It’s about empowering yourself with knowledge and making informed choices to support your ocular surface health long-term.
Recommended Video
Understanding tear film dysfunction is the cornerstone of effectively managing dry eye syndrome. By recognizing the intricate roles of the lipid, aqueous, and mucin layers, and accurately identifying whether the primary issue is aqueous deficient dry eye or evaporative dry eye, we can move beyond temporary fixes to truly restore ocular comfort and clarity. This deeper understanding, combined with a biohacking mindset, paves the way for comprehensive, evidence-informed strategies that foster long-term eye health and clear vision.
What is tear film dysfunction?
Tear film dysfunction refers to an imbalance or instability in the eye’s natural tear film, leading to inadequate lubrication and protection of the ocular surface.
- It is the primary underlying cause of dry eye syndrome, rather than solely a lack of tears.
- This dysfunction can involve issues with the quantity or quality of any of the tear film’s three distinct layers: lipid, aqueous, or mucin.
- When the tear film is compromised, it fails to properly hydrate, nourish, and protect the eye, causing irritation and visual disturbances.
How does tear film dysfunction cause dry eye symptoms?
Tear film dysfunction causes dry eye symptoms by increasing tear evaporation, reducing lubrication, and promoting inflammation on the eye’s surface.
- An unstable lipid layer, often due to meibomian gland dysfunction (MGD), allows tears to evaporate too quickly, leading to dryness.
- Insufficient aqueous production (aqueous deficient dry eye) means there aren’t enough tears to wash away irritants and keep the eye moist, resulting in friction.
- Breakdown of the mucin layer can cause tears to unevenly spread across the eye, creating dry spots and blurred vision.
- The resulting chronic dryness and irritation activate inflammatory pathways, further damaging the ocular surface and exacerbating symptoms.
What are the benefits of addressing tear film dysfunction directly?
Addressing tear film dysfunction directly leads to more effective and sustainable relief from dry eye symptoms, improving comfort and overall eye health.
- Targeting the specific tear film layer(s) involved—lipid, aqueous, or mucin—allows for precise and personalized treatment.
- It can significantly reduce chronic eye irritation, burning, and grittiness by restoring the natural protective barrier.
- Improved tear film stability often leads to clearer and more consistent vision, as the eye’s refractive surface is smoother.
- Long-term management of tear film health helps prevent potential complications like corneal abrasions or infections.
Are treatments for tear film dysfunction safe, and what are the main considerations?
Treatments for tear film dysfunction are generally safe when prescribed and monitored by an eye care professional, but considerations vary based on the specific therapy.
- Common treatments, like artificial tears and warm compresses, are very low risk and primarily aim to supplement or improve tear quality.
- Prescription medications, such as anti-inflammatory drops or secretagogues, may have mild side effects like temporary burning or redness, which are usually transient.
- In-office procedures, such as LipiFlow for MGD, are minimally invasive but require careful patient selection and adherence to post-procedure instructions.
- It’s crucial to discuss your full medical history and any existing eye conditions with your doctor to ensure the chosen treatment plan is appropriate and minimizes potential risks.